Personal well-being equips us to better care for patients
Posted on January 28, 2021 by Carol McPhail

To understand the importance of well-being, you first have to understand what the opposite looks like in a colleague.
“You see the fun starting to fade,” explains John Anaya, M.D., a third-year internal medicine resident. “If you love medicine, it should be fun. Especially here (at USA Health), it’s easy to have fun at work.”
Even in the best of programs, the stress of transitioning from a medical student to a practicing physician can be intense, particularly during the internship year. Long hours in the hospital can produce fatigue that, if not addressed, can impact performance and lead to burnout.
“If you’re exhausted, you’re not going to gain the information you need. I don’t learn well when I’m tired or fatigued,” said Farheen Surtie, M.D., Anaya’s wife and fellow resident. “It’s very important that programs focus on well-being.”
The USA Office of Graduate Medical Education just kicked off a well-being program based on the eight dimensions of well-being: physical, emotional, occupational, spiritual, intellectual, environmental, financial and social. The plan is to encourage participants to complete a personal well-being self-assessment as a baseline and move on to work on healthy habits related to sleep, diet, exercise, routine exams and more. It’s an effort encouraged by the Accreditation Council for Graduate Medical Education, which has called on GME programs nationwide to address well-being along with other aspects of resident competence.
“There are many national stakeholders, from the American Medical Association to the National Academy of Medicine to the Joint Commission, who recognize that to provide the safest and highest quality patient care, we as providers need to be healthy and have an understanding of personal well-being and our responsibility for maintaining it so that we can take care of patients,” said Carole Boudreaux, M.D., associate dean for graduate medical education. “We encourage all GME programs that do not have a defined and implemented well-being program in place for residents, fellows and faculty to adopt this program.”
The first steps include selecting a resident or fellow and faculty member to be the champions for well-being in their departments, and engage the program coordinator. Have the residents and fellows complete an assessment of their existing habits as a starting point. Then, plan the curriculum for module 1 (physical well-being), and kick it off with a speaker or a TED Talk. A host of healthy lifestyle resources can be found at mayoclinic.org and verywellfit.com for participants to develop their physical well-being plans.
The Appalachian Trail Virtual Challenge promoted by USA campus recreation will provide an opportunity for some friendly competition for the physical well-being dimension. The challenge calls on teams from the various residency and fellowship programs to work together to log the 2,190 miles between Springer Mountain in Georgia and Mount Katahdin in Maine as if they were walking the actual AT. The JagFit@South team plots the teams’ locations along the trail weekly, and the first team to walk the 4.3 million steps wins the race.
“Simply getting USA and USA Health employees walking daily is so important to help relieve the stress and anxiety of their daily lives during normal times,” said campus recreation director Brian Allred. “It is even more important during this pandemic.”
For first-year internal medicine resident Taylor Cook, M.D., the best way to re-energize is by spending time outdoors, whether it’s swimming in her backyard pool in west Mobile, biking or visiting a park or beach. “It reminds me there are bigger things than myself and a whole world outside of the hospital,” Cook said. “One bad day doesn't affect the world the way it does you. The world keeps on moving regardless of that one mistake you made or the answer you didn't know.”
The Oklahoma native said she chose USA for residency training because of the supportive family atmosphere. “I think the program here does a great job of promoting well-being and making sure we make that priority in our lives,” she said.
But if stress and fatigue begin to take their toll, reaching out to a mentor or chief is a good idea.
Two to three weeks into his internship year, Anaya contacted his chief resident and said he felt overwhelmed. “I had a long conversation with him about things, and he made sure I had what I needed in order to get back on the rails,” he said. “We scheduled a little vacation not too long after that, and with a little bit of rest and little bit of coaching, everything perked up.”
One of the toughest rotations is working “wards” in the hospital, which usually means six days a week starting at 6:30 or 7 a.m. and ending 10 to 12 hours later.
After working wards for four to five months straight during COVID, Surtie became exhausted. “I don’t even think I noticed it myself,” she said. “I had a meeting with my program director one on one. They adjusted my last month of wards because I had been on inpatient for so long.”
Surtie and Anaya say that being on different rotations from each other helps them to cope. When Surtie was on wards for months, Anaya picked up the slack at home. “I did my best to have dinner ready when she got back,” he said. “When I’ve gotten a little tired, she has done the same for me.”
Also, scheduling a daily sit-down supper gives the couple a chance to unwind and connect before turning in between 10 and 11 p.m.
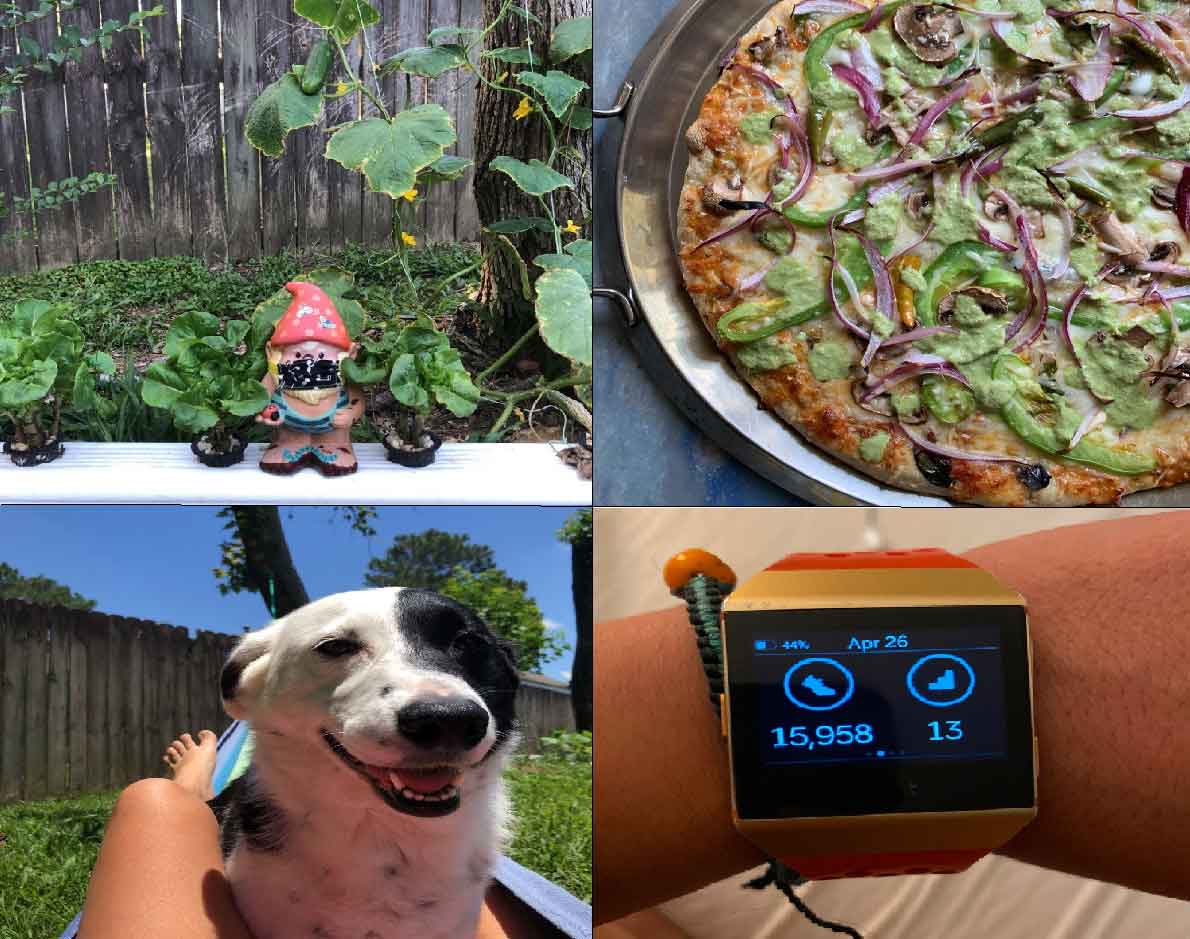 Earlier this year, they found an outlet in GooseChase, a well-being challenge in which
internal medicine residents participated in healthy activities and shared their experiences.
Anaya recreated the “Wilson” scene from “Castaway.” In another video, he added humor
by filming himself doing lunges.
Earlier this year, they found an outlet in GooseChase, a well-being challenge in which
internal medicine residents participated in healthy activities and shared their experiences.
Anaya recreated the “Wilson” scene from “Castaway.” In another video, he added humor
by filming himself doing lunges.
Surtie and a few friends contributed a skit that was set to a tune from the Backstreet Boys. “Our competitive streak came out,” she said. “And it was something to do outside of medicine.”
Other internal medicine activities have included a mindfulness session and creating a gratitude “tree” for the resident lounge, a senior skip day in which attendings cover for residents so they can have a socially distanced get-together, and a superhero day as a thank-you to frontline workers. OB/GYN, meanwhile, has granted half-days off for residents to allow them to keep personal health appointments and recharge.
Eating healthier is another important tenet for sustaining physical well-being. USA Health physicians always have been able to grab free meals and snacks from designated refrigerators at the hospital cafeterias, and recent changes have resulted in a wider variety of less processed offerings. “You can pick a soup, salad, sandwich or little snacks such as grapes, crackers and cheese,” Anaya said.
Next year, Surtie and Anaya will serve as two of the three internal medicine chiefs. Anaya, who is planning a career in nephrology, is considering taking on well-being as one of his projects as a chief.
Allison Beckett, M.D., a fifth-year surgery resident, praised the fact that well-being has become a much more mainstream topic for many programs. “For me, personal well-being is more so a state in which you are happy doing whatever it is that brings you fulfillment and happiness,” said Beckett, who will start a cardiothoracic fellowship next fall. “If you ask any one of my co-residents, they’ll tell you I’m a work horse. I am most myself when I stay busy working.”
Beckett likes to savor the “little things,” such as getting a favorite cup of Starbucks on the way to work. She finds the most joy, though, spending time with her husband, Mina, and daughters, Claire and Isabelle. “I find myself always showing pictures of how fast they are growing to my co-residents and attendings,” she said. “While fellowship will bring its challenges, my two girls and my husband will keep me going.”
